Doctors With Mental Health Issues – Doctors now have a harder job than ever. Given the health situation in 2016, providers must understand how to manage the confusion arising from issues such as payment models and new government regulations, while managing chronic patients and coordinating care and communication among multiple providers.
These challenges seem difficult, but they also show opportunities for doctors to improve patient care by better understanding and targeting the patients they serve, improving communication and education, and using technology to achieve their goals. Read on to see some of the key challenges facing doctors today.
Contents
- 1 Doctors With Mental Health Issues
- 2 New Program To Solve Mental Health Issues Of School Students
Doctors With Mental Health Issues

Nearly 25 percent of US medical doctors say they are not well prepared to care for patients with multiple chronic conditions, according to a new 10-state survey by the Commonwealth Fund, which promotes effective health care systems. Despite having a younger population than many other developed countries, the US has a higher percentage of patients with multiple chronic conditions.
Of Doctors Believe Mental Health Issues, Depression Will Be The Biggest Non Covid 19 Issue As A Result Of The Pandemic
About half of adults – 117 million people – have one or more chronic health conditions, which cause 7 out of 10 deaths each year. According to the Centers for Disease Control and Prevention (CDC), treating patients with chronic diseases accounts for 86 percent of our nation’s health care costs.
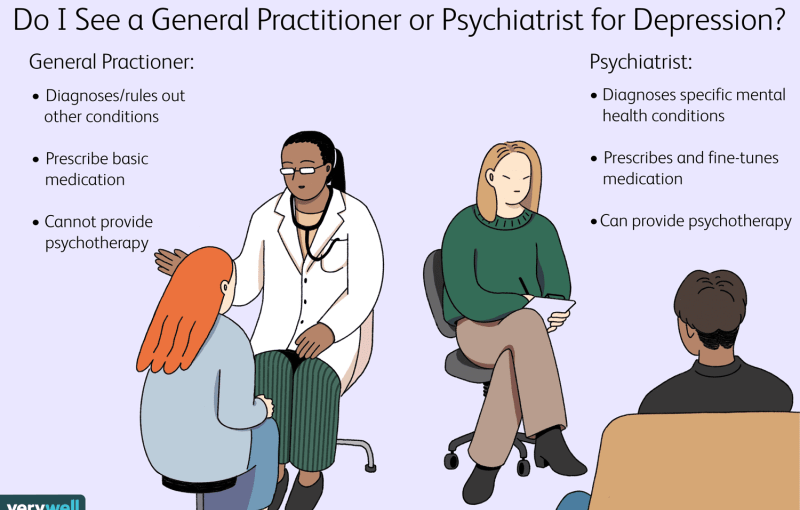
The same study found that 84 percent of US general practitioners say they are not well prepared to treat patients with severe mental illness. About 1 in 25 US adults — 10 million — will have a serious mental illness in a given year that significantly interferes with or limits one or more important life activities, the National Institute of Mental Health reports.
This issue affects all doctors because “a patient’s mental state greatly affects their ability to survive and fight disease,” writes Richard Robinson, M.D., of KevinMD.com. “Anxiety and depression can make patients more vulnerable to harmful stimuli, so identifying these symptoms can help better understand the patient’s current situation.”
According to Commonwealth Fund research, only one in three doctors say they are notified when a patient is admitted to the emergency department or discharged from hospital. (Compare this to the Netherlands, where 69 percent of doctors reported that they were often informed when prescribing.)
Mental Hospital: Treatments Offered, How It Works
The lack of coordination of care and communication has not only caused frustration and confusion for patients, but can lead to readmissions, suggests Ilene MacDonald, editor of FierceHealthcare.com. Because of the Affordable Care Act, hospital readmission rates will become even more important for doctors going forward, as readmissions can lead to financial penalties and gaps in care. Strategies to improve communication include using reporting methods with patients and careful follow-up—again a good way to avoid judgments of misconduct.
Medical Economics says the cost of information technology in medicine has increased significantly in recent years and is not expected to decrease anytime soon. According to HealthcareIT News, more than 80 percent of US physicians now use EHRs. However, keeping IT and support costs down is a major concern for many physicians. More practices are moving to cloud-based EHRs, billing systems and patient education systems to avoid the upfront costs of new software and computers. (For more on this, see our post on cloud computing for doctors.)
Digital health tools that impact patient engagement will continue to be a hot topic in 2016. The IoT healthcare market is expected to reach $117 billion by 2020. The adoption of wearables increased by 60 percent in 2015, and half of the patients were hospitalized in the region. Last year, they started using wearables after a hospital stay, according to health data company Health Catalyst.

Physicians need to understand how different patient populations and generations use technology, whether it’s wearable devices or online patient education, and consider how to keep patients actively engaged in technology that can improve their health.
Data And Drivers Of Doctors’ Mental Health — Burnout And #mh4docs At #ranzcp2019
Other challenges facing physicians in 2016 include getting paid what they deserve as payment models shift from fee-for-service to fee-for-performance, the effects of the merger of the nation’s largest health insurance companies, and balancing the risks and benefits of independence versus employment.
We use cookies to ensure you have the best experience on our website. If you continue to use this site, we’ll assume you’re happy with it. OkPrivacy Policy If you’re a healthcare professional and have concerns about your mental health, go to /frontline for screening and resources and support. If you are experiencing a mental health crisis, call 1-800-273-TALK (8255) to access the 24/7 Crisis Center or text MHA to 741741 to reach a trained crisis counselor 24/7.
Throughout the COVID-19 pandemic, Mental Health America (MHA) has seen an increase in depression, anxiety, loneliness, and other mental health issues. COVID-19 has had a devastating impact on the nation’s mental health, especially for those facing the challenge of fighting the virus.
While many in the US deal with the fear and uncertainty of COVID-19 in their homes, critical workers, including healthcare workers, are exposed to the virus every day. Health care workers experience conditions that have been compared to a war zone, often seeing the first effects of an epidemic as it spreads throughout society. It is important that we provide resources to help health professionals address the impact of their work on mental health.
The History Of Mental Illness: From
From June to September 2020, MHA conducted a survey on mhascreening.org to listen to the experiences of healthcare workers during the COVID-19 pandemic and create better tools to support their mental health as they continue to provide care.
The following analysis is based on responses from 119 health professionals who participated in the MHA Screening (mhascreening.org) survey between June 1 and September 1, 2020.
The majority (70 percent) of respondents were white, followed by black or African American (10 percent) and Hispanic or Latino (8 percent).
The largest groups of respondents were other health professionals (30 percent) and nurses (22 percent). Nineteen percent of respondents listed their occupation as other, including mental health professionals, social workers, and pharmacy workers, among others.
Young Doctors At High Risk Of Mental Health Problems
52 percent of healthcare workers surveyed were not known to be in direct contact with COVID-19 patients but could be exposed. 28 percent have worked directly with COVID-19 patients.
Nurses are more likely to report exposure to patients with COVID-19 than the general population responding to health services. Among nurses, 41 percent reported working directly with COVID-19 patients and 49 percent reported they could be affected.
No, but I may be vulnerable to COVID-19. (eg in rooms with COVID-19 patients, work on the same floor as COVID-19 patients, use the same cafeteria, etc.)
However, the majority (73 percent) of health care workers who responded had not previously been infected with COVID-19 at the time of the survey. 10 percent had a confirmed or suspected case of COVID-19, and 17 percent were unsure.
Healthcare Professionals And Substance Abuse
The MHA asked the health workers: “Of the following feelings, which have you had most often in the past three months? Mark everything that works.”
Stress was the most commonly reported feeling, with 93 per cent of healthcare workers reporting that they had always been stressed in the past three months. This was followed by anxiety (86 percent), depression (77 percent), tiredness or fatigue (76 percent), and feeling overwhelmed (75 percent). Fewer people expressed gratitude, hope, and pride, although almost a third (31 percent) reported being grateful often.
Which of the following emotions have you felt most often in the past three months? Search for all that works.

MHA also asked health professionals: “In the past three months, have you experienced an increase in the following symptoms? Mark all that apply.”
Pdf) Fitness To Practise For Doctors And Medical Students With Mental Issues In Malaysia
Healthcare workers are the most likely to report being emotionally exhausted in the past three months (82 percent). This was followed by sleep disturbances (70 percent), physical fatigue (68 percent) and fear caused by work (63 percent). More than half of healthcare workers have reported changes in appetite (57 percent), physical symptoms such as headaches or stomach aches (56 percent), questioning their work style (55 percent), emotional exhaustion (52 percent), and increased awareness, anxiety. , or attention. exposure (52 percent).
Have you increased any of the following in the past three months? Search for all that works.
When asked about emotional support, the largest group (39 percent) of health workers indicated that they did not feel they had enough emotional support. Another 26 percent were not sure if they were getting enough emotional support.
Nurses were less likely to report having adequate emotional support than other health professionals. Of the nurses surveyed, 45 percent reported that they did not have enough emotional support, and 24 percent were not sure.
New Program To Solve Mental Health Issues Of School Students
More than half of health workers receive emotional support from family (57 percent) and friends (53 percent). Most health workers also reported receiving emotional support from colleagues (38 percent).
When asked to choose their top three work-related stressors, 61 percent reported uncertainty about when things would resolve or return, and 54 percent.
Issues with mental health, women with mental health issues, homeless with mental health issues, adults with mental health issues, students with mental health issues, dealing with mental health issues, person with mental health issues, employees with mental health issues, living with mental health issues, help with mental health issues, celebrities with mental health issues, struggling with mental health issues